Insulin and Glucagon - How They Regulate Blood Sugar Levels
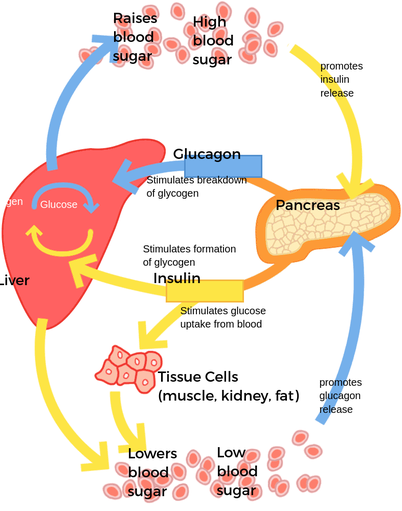
Glucagon and Insulin are the two powerful hormones that regulate blood sugar levels in the human body. They also work together to help prevent diabetes. However, there are some important differences between the two hormones.
Glucagon is a powerful regulator of blood sugar levels
Glucagon is an insulin-like peptide hormone that increases blood glucose levels and prevents dangerous hypoglycemia. It is produced by the pancreas and is released when blood glucose levels are low with Non-invasive Screening Products. Glucagon works in concert with other hormones such as insulin to control blood sugar levels.
The pancreas is a glandular organ located in the abdomen. It is surrounded by the stomach and intestines. It secretes hormones that regulate blood glucose levels. These hormones also send messages to organs, skin, and muscles.
The pancreas produces several hormones, including insulin, glucagon, and amylin. These hormones help maintain blood glucose levels by promoting the breakdown of fat in fat cells and by inhibiting the production of glucose in liver cells. In addition, the hormones cortisol and growth hormone help regulate blood glucose levels.

image source: https://www.pinterest.ph
Glucagon increases glucose uptake in the tissues
Glucagon is a hormone secreted by the pancreas that helps maintain blood glucose levels in a narrow range. It stimulates glycogenolysis, which breaks down stored glucose into energy. The opposing actions of glucagon and insulin maintain glucose homeostasis. When glucagon interacts with insulin, glucose is released from the liver. The liver stores glucose as glycogen. When the glucose level falls, the liver starts glycogenolysis to make glucose again.
Research on this hormone and its receptor has been ongoing since 1977. This study is aimed at understanding the role of the brain-derived neurotrophic factor in glucose metabolism. Glucagon is a peptide hormone, which stimulates the breakdown of stored glycogen into glucose. It is produced when blood glucose levels fall. The release of glucagon is suppressed by insulin, which triggers glucose uptake into insulin-dependent tissues.
Glucagon decreases mobilization of lipids in adipocytes
Glucagon may have an important role in acute regulation of lipid metabolism, but the direct effect of glucagon on lipid metabolism has been difficult to ascertain. Some studies suggest that the lipolytic effect of glucagon can be counteracted by insulin. However, further studies are needed to assess the role of glucagon in lipid metabolism like in Point of Care Testing.
Glucagon may influence lipolysis in adipocytes, which is mediated by perilipins on the surface of lipid droplets. This results in the release of fatty acids (FFAs) and glycerol. Glucagon has been shown to inhibit glycolysis, to stimulate gluconeogenesis, and to reduce triglyceride (TG) secretion.
Glucagon inhibits b-oxidation by phosphorylating acetyl-CoA carboxylase, a key enzyme in fatty acid synthesis. It also stimulates the production of PPARa, a gene that promotes b-oxidation genes. In vivo experiments suggest that glucagon may be essential for lipid metabolism.

image source: https://www.pinterest.ph
Diabetes mellitus is caused by b-cells
Historically, the view of diabetes mellitus as an autoimmune disease was believed to result from the destruction of insulin-producing b-cells in pancreatic islets. But recent studies have shown that the disease can be triggered by other factors with Blood Glucose Monitor.
Type 1 diabetes mellitus (T1DM) is an autoimmune disease. This is believed to result from the destruction of insulin-producing cells in the pancreas by autoreactive T cells. Alternatively, it is thought that the disease might occur as a result of viral infection, b-cell degeneration or increased pancreatic adiposity. However, it remains unclear whether any of these factors play a significant role in the pathogenesis of T1DM.
Single-cell analysis techniques have revealed a widespread b-cell population in healthy pancreas. During disease progression, the b-cell population has become heterogeneous, with different oligodendrocyte phenotypes leading to different levels of autoimmune reactions.


































