Brain metastases (BrM) are the most common intracranial tumors, mainly originating from lung cancer (40–50% of cases), breast cancer (15–25%), and melanoma (5–20%). Despite treatment with molecularly targeted therapy, immunotherapy, stereotactic radiotherapy, or conventional surgery, their median survival is only 5–10 months. This emphasizes the need for a deeper understanding of BrM biology to develop more effective treatments.
The vascular system is a key component of the tumor microenvironment in BrM and plays a critical role in regulating the metastatic dissemination and progression of the tumor. However, the heterogeneity of the major components of the BrM vasculature (endothelial cells and mural cells) is still poorly understood.
On January 18, 2024, researchers from the University of Lausanne, Switzerland, published a research paper in the journal Cancer Cell entitled "Interrogation of endothelial and mural cells in brain metastasis reveals key immune-regulatory mechanisms".
Recent analysis of brain metastasis patient samples has revealed the importance of the brain tumor microenvironment (TME) in regulating disease progression in primary and metastatic brain malignancies. The vast complexity of the TME in BrM is being revealed, with immune-cell landscapes being a key focus to date. However, a similar comprehensive mapping of the vascular lumen in human BrM is currently lacking.
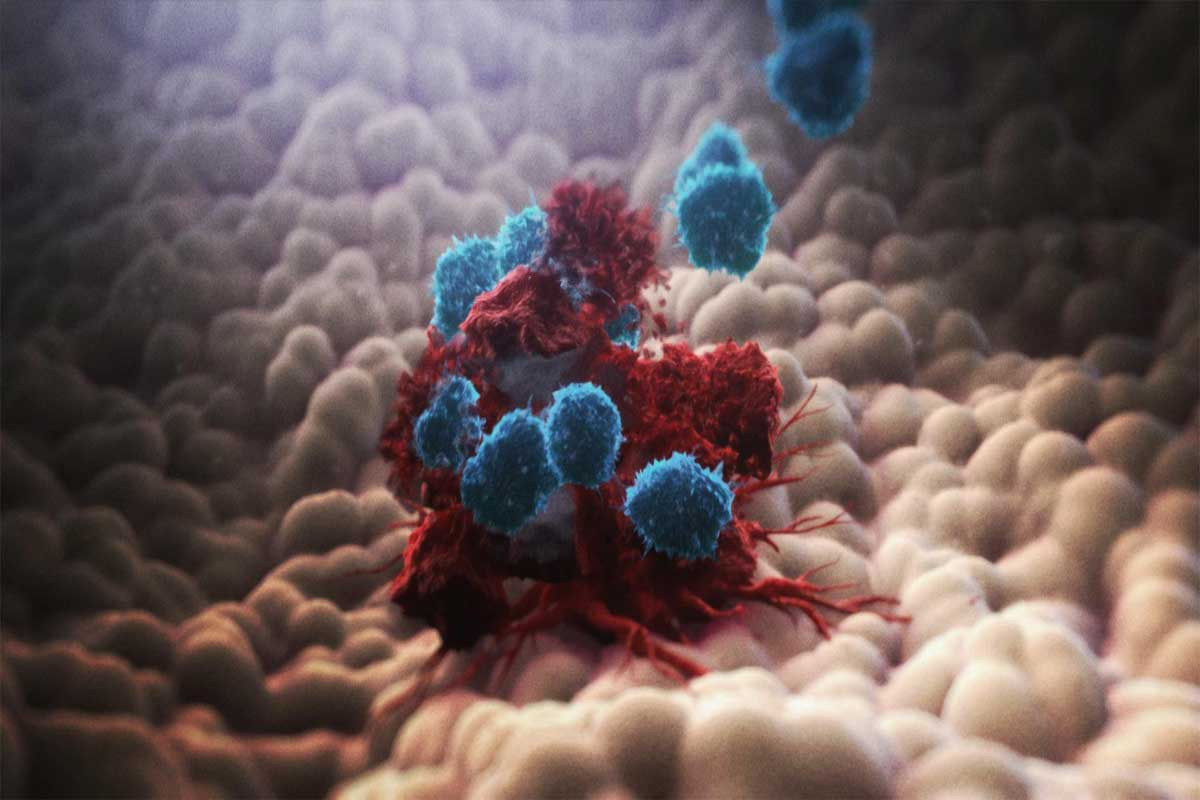
The blood-brain barrier (BBB) is composed of endothelial cells (EC), mural cells, astrocyte endfeet, and tightly associated microglia. The tight junctions formed by endothelial cells act as a selective barrier, allowing essential nutrients to enter while protecting the brain from pathogens and toxic substances. However, metastatic cancer cells can cross the BBB by a different mechanism, and after these cancer cells colonize the brain, they alter its vascular system to form a blood-tumor barrier. While this abnormal vascular system may infiltrate peripheral immune cells, including CD8+ T cells, it does not induce a lasting immune response.
In this study, the research team performed an in-depth analysis of key components of the brain tumor vascular system. Single-cell RNA sequencing, bulk RNA sequencing, and spatial tumor microenvironment imaging analyses were performed on vascular cells from human and mouse brain metastases and non-tumor brain samples, and preclinical studies were conducted using the BrM model to try to answer the following questions:
* What is the heterogeneity of endothelial and mural cells in BrM?
* What are the structural and molecular alterations in these vascular components associated with BrM?
* How can we therapeutically target the BrM vascular system?
This study provides effective therapeutic strategies for these aggressive tumors through a deeper understanding of BrM biology.
Analysis of this study revealed significant differences in gene expression patterns between endothelial and mural cells in brain metastases and the same cells from non-cancerous brain tissue. This suggests a variety of aberrations in the brain tumor vasculature, including problems with intercellular junctions and adhesion of endothelial and mural cells, reflecting the leakiness of the tumor vasculature, which inhibits anti-tumor immune responses or induces the suicide of T-cells targeting cancer cells.
The team integrated these experimental data with mouse models to create a platform for discovering therapeutic targets against the vascular system of BrM. An immunosuppressive molecule, CD276, was discovered, that is particularly abundant in endothelial and mural cells of brain metastases and could serve as an emerging target for cancer immunotherapy. CD276 is known to inhibit T cell proliferation, support immune escape from cancer cells, and correlate with a poor prognosis in cancer patients.
The team further demonstrated that antibodies targeting CD276 inhibited brain tumor growth and significantly prolonged survival time in a mouse model of breast cancer. In addition, this treatment altered the vascular structure at the molecular level and promoted the entry of killer T cells into the tumor.
In addition to identifying CD276 as a promising therapeutic target for brain metastases, the study provides important insights into the complex interactions between the vascular system, immune cells, and cancer cells, which could have translational implications for the development of therapeutic interventions against brain metastases.